Hi and thanks for taking the time to read and hopefully reply to my post.
I am a 30 year old female who is slim and fit but with a :
'Acute prolapsed intertebral disc to the left at the L4/L5 with L5 sciatica'
I have had this for over 12 month, I've seen a physio and a chiropractor all without success. The pain comes and goes, there are good days and bad. Since my discetomy has been scheduled (19th April 2012) the pain has become bareable (Unless I am flying to meetings for work)....this combined with the fear I have for the actual operation itself, I am wondering whether or not to go ahead.
I am concerned with the possible complications (incontinence and dropped foot) and I am also concerned about how I will feel afterwards - in the short term.
I have never had an operation before, so need some truthful and open first hand experiences on what to expect. I also need to know if this is right for me.....I have been advised that the injection in my case is unlikely to be more than be 30-40% successful but the operation is likely to be 90% successful My surgeon is a Mr Jonathan Lucas so any reviews or experiences with him would be great.
Thanks for your thoughts on this – Sometimes input from those who have ‘been there, done that’ can be vital….
I am in exactly the same predicament as you are now, I have had problems with my back and my right leg at L5/S1 for approximately 7 months. I was laid up on my living room floor for 5 weeks before i was admitted into hospital and received an epidural steroid shot.
This got me back on my feet, but i still have numbness, particularly in my toes and side of the foot and cramps all up my leg.
I have been offered the op 3 times now and declined, mainly for fear of the anaesthetic. However i have now found the endoscopic miss method that is conducted in an aware state and my fears are now towards whether or not the operation will be a success and the complications involved in the procedure.
Im just one big bag of nerves at the moment and i havent even had a date for any surgery if required!
i think its a fear that we all have over whether the op will be a success. More so as its your back and pivotal for everything.
Im worried that if i leave it it may get worse and i may leave it too long for the surgery to have any effect, but on the flip side im worried that something will go wrong with the surgery!
I got all my paperwork through today and the my pre surgery appointment is Thursday (5th April 2012) and I am really freaking out.
The pain is so much better than it was two weeks ago, to the point where i am not even taking pain relief now....After reading reviews on here I am seriously thinking of cancelling....
Is it really possible that after over 12 months of pain it can suddenly get better? Or is it a physiological thing that because i know I am due to have an op my body is handling it differently?
It sounds like you have a worse case than me Charlie....I haven’t taken time off work for it...although i have spent the last 12 months pretty much standing at my desk and i spent a 6 hours of a 12 hour flight standing up!
I really don’t know what to do....Massively freaking out...
Hi and welcome
The pain can get better on it's own, the disc may move or shrink. If you don't need painkillers at the moment then you really don't need an op right now do you?
Hi Cascara,
I agree with you, but the problem is when I do have pain I can't sit or do anything....be it lay on the sofa and watch tv or get on the bus to go to work...it gets to the point where I break down and am in bits..then I will have a couple of "good" weeks....then it's back....(excuse the pun!)...and this has been going for more than 12 months, and it's mostly on...
I had an MRI in September and at the end of march this year...they were both the same with no improvement.
I'm so worried that if I have the op it will be worse as it seems people on here are still having issues and additional issues after the op.....I have really worked myself up about this and mentally it's causing me a lot of anxiety...
Hi there,
I just wanted to share this link, which you may have seen on another thread [url]EuroSpine - Sciatica[/url]. It was given to me by a surgeon who wanted me to have an informed choice. I was eligible for surgery because my (significant!) pain matched the MRI scan. I decided against surgery and was lucky to have an exceptionally good NHS Physio who helped enormously.
I know you mentioned that you hadn't had success previously with a Physio, but it must be good that you are able to get pain free periods of time and I wonder if perhaps it would be worth discussing with a Physio your posture and track back things that you are doing with them that are perhaps causing your flare ups. They may be able to help you significantly reduce your reoccurrences by correcting your posture and advising on lifestyle e.t.c. I hadn't realised that I sat very poorly - in a C shape and this was putting pressure on my discs, the Physio helped correct this and I now use a lumbar roll. We sometimes don't realise how poor our posture is.
I wouldn't worry too much about the MRI scan (easier said than done, I know!) I read somewhere or someone said we always "treat the man not the scan" and people with the same injury can have very different degrees of pain.
Spinal surgery is a very serious business and for me the evidence was too conflicting to go ahead, although at times in awful pain I was known to cry out for them to take me under the knife. I like to read the stories about sports people who have had this injury and bounced back without surgery - like Steve Redgrave and Kelly Southerton, both determined to continue with their sports and therefore not wanting surgery.
Like you I was worried about potential for adverse effects and I was advised that when it comes to sitting down, surgery may make the problem worse, so that was my decider. I have a predominately sitting and driving job.
It really has to be a good thing that you are able to get pain free periods and may well be worth seeking advice on how to maintain that first? Do you keep a diary on the things that you do that cause a flare up? That may help identify things to avoid/adjust too?
This is a long journey and my physio has advised me it can take up to 2 years to recover fully whether you have surgery or not and along the way you can have flare ups whichever route you have taken.
I hope my ramblings have helped.
Good luck!
Jayne x
Hello pain and welcome!
Because of your doubts over whether to go under the knife or not, you really should not go ahead at this time, you are only 30 years old and may have a long time to regret your decision. It also seems you need far more information too!
You are right to be worried about discectomy, it is a very serious and destructive procedure which requires an excelent and (above all) a caring Surgeon to successfully pull it off, without causing substantial collateral damage!
I am not aware of Mr. Lucas, so he may well be a good Surgeon, but I am concerned about speed he has gone for surgery and the 90% success rate he quoted you, as I have spent over 4 years throughout the UK looking for confirmation of this figure, without any success!!
I would agree with Cassie, if you can find a way around working without drugs, with or without the help of therapists, then don't have this destructive procedure yet! You are too young and active!
If you do decide to go down the surgical route, check out Minimally Invasive Spinal Surgery (MISS) or Minimal Access Surgery (MAS) before deciding on discectomy.
Here are some links for you to compare the differences between what you have been told and MISS.
Best wishes
SPINELF
I am seven weeks post op. I would delay the operation and look at every other alternative ie core strengthening etc unless you are in acute pain and you dont feel you can cope anymore having tried everything.
Believe me the procedure is invasive, prepare to take a big hit on your body without any guarantee of success.Its quite easy to get hung up on the results of an MRI scan.
The people who appear to benefit most are those who go in with serious sciatic pain and get almost instant relief. If you are like me (and it sounds as if you are) with an ongoing on /off history and an MRI scan to match you almost pressure yourself into getting it done.
btw my sister had 12 months like you and her pain stopped the day before the operation- perhaps your body is trying to tell you something.
Hi Doog,
I read the post between you and Ricky and to be honest it was this that put the fear of god into me....
I am seeing my surgeon on Thursday for the pre op consult but have already emailed his PA stating I am having doubts.
Doog is it really horrendous after? How are you now? Was you recovery and experience post of typical, or were you unlucky?
I keep thinking about how I feel when it's bad and wonder if I was like that t this very moment whether my doubts would be so strong...
I really appreciate your thoughts, all of you
Heidi
Hi Heidi
Please dont let Ricky's thread put you off from making an impartial decision. Its fair to say that with the both of us having the op within a few days of each we found a common purpose and that was access through the thread to post our daily thoughts..good, bad and sometimes very detailed.
For me Ricky's thread was a great comfort in that I had someone to relate to and perhaps post detail that I wouldn't ordinarily do.
My issue is more one of frustration. I was into my sports and the injury that led to the operation was work related and happened nearly 4 years ago. My sciatica was up and down throughout that time. I tried everything possible but the surgeon told me things would never improve without an operation, so I took his word for it. For example I was into cycling 100 miles in a day. Now that sort of physical activity isnt normal but I wanted to be able to do that without pain. I always said that if I led a sedentary lifestyle I wouldnt have had or needed the operation.
I think half the problem with modern life is the urgency for us all to get back to normality as quickly as possible. That means work,driving, sports etc. However if you look at seven weeks in the big picture of the operation its nothing really and I guess we are still finding our feet, Ricky probably has age on his side so his progress may be quicker
On a personal level I need to slow things down, I tried to come off the meds too early, tried to walk too far and just over did things. There was an 82 year old chap in the bed next to me who had an instant recovery. I saw him two weeks later and he has no pain.
You need to have an honest and open chat with your surgeon, I would like to think they wouldnt operate unless they thought they could help you.However please explore all other options, physio, pilates etc. My decision was made over 4 years (since I joined this forum) I saw 2 surgeons, one said no, the other said yes on both occasions that I saw him. Every physio I saw said no....two consultants said no, both surgeons and consultants didnt really have a good word to say about the physios......its a mine field
I wish you all the best in your decision.
Thanks Doog.
I feel that I have tried nearly everything and I think that is the problem....I am at my wits end....especially since the pain today is back....sigh.
My family do not think that i am in the right place mentally for this op, and they are probably right. I am meeting my surgeon tomorrow morning and will ensure I ask everything that needs to be asked and make an informed decision.
Sometimes the internet is a wonderful place to gleam information, other times it scary.
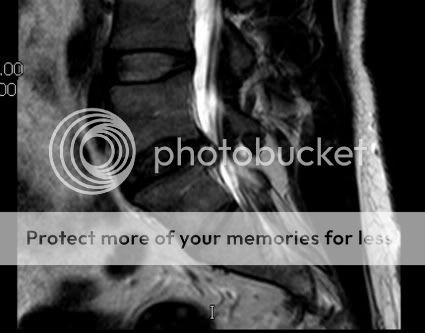
I have attached to this my MRI scan, I know each person is different, but how does my prolapse compare to what you had?
Thanks again for your thoughts.
Hi Heidi,
I really feel for you and know that this is a really hard choice to make.
Please try not to get too hung up on the scan - I know I did and would go to sleep with that image in my mind - and yes mine looked just like yours only at L5/S1. It just adds to the distress and as I said on the other thread my Physio says it is far easier to treat people with sciatica who haven't had an MRI scan even though the cause is still probably a prolapsed disc.
I really think you need to concentrate on the good periods where you have less/no pain than the bad painful times. There must be something that you do, positions that you get in that reduce the pain, if you can discover what those are, or conversely what positions/activities cause you pain then you stand a good chance of reducing your recurrences and therefore recovery. I did this with my Physio.
Perhaps set yourself a deadline with the surgeon tomorrow - perhaps if no improvement in 3 months time reconsider. The fact you are able to get pain free really makes me believe surgery is not needed at this moment.
I don't know if you have seen the McKenzie book "Treat Your Own Back" but in there he states that even if you only have 10 minutes pain free a day, the fact that you are able to get pain free, means that you stand a good chance of an exercise based recovery. I know there are sceptics about the McKenzie method, but I like to think it worked for me.
You may have to accept that you have to make some lifestyle changes to help the recovery period, but these are usually manageable. For example I never sit for longer than 40 mins at a time - this used to be embarrassing in meetings, but now I just say to the Chairman I need to get up for a little walk around every so often because of my back. I had one Chairman make everybody stand and he thought it was an excellent idea!!!
For car journeys the same - I just plan frequent stops on a long journey and get out for a couple of minutes and walk around and I have gone from a sedentary lifestyle to doing at least a 30 minute brisk walk a day. All in all my injury has actually made me a much healthier person!!
For me the evidence for surgery was too conflicting and there really is no turning back.
Are you really sure you have tried everything? Are you still with a Physio, sometimes it can seem like they make things worse before better. Have you tried any of the nerve drugs like amitriptyline, gabapentin or pregabalin (although they can have side effects). TENS machines work for some. Is it worth taking a bit of time off work just to get yourself back on track?
Good luck with the surgeon tomorrow - please let us know how you get on.
All the best.
Jayne
ouch that looks sore, its obvious what the problem is but not being an expert I cant really comment further:) All I can do is show you my scan. With mine the surgeon simply said the prolapse at 1cm would never go away or shrink back hence I went for the operation. Your surgeon may say the same, if not ask him directly 'will it ever go away?'
At my pre-op the nurse said that few patients came in in absolute agony, many were mid to long term sufferers who just wanted a better quality of life.
Heidi
one more thing that influenced my decision (after reading Jaynes post about lifestyle changes)is that I work for the emergency services. I wasn't exactly being pushed into a corner but naturally they wanted to know if there was a long term solution.
They paid for me to see the surgeon, so in a way I was also looking at saving my career.
best of luck
With mine the surgeon simply said the prolapse at 1cm would never go away or shrink back hence I went for the operation. Your surgeon may say the same, if not ask him directly 'will it ever go away?'
Hi Doog,
How did he know it would never go away though? My surgeon said in all honesty, they weren't actually clear what happens. There is a theory they dehydrate and pull back, other theories that fragments are reabsorbed or that macrophages recognise that the disc is in the wrong place and "gobbles it up"!!!.
How long it takes to do this seems to be anybody's guess!!
I really wish there was an expert contributing to this site!!
It would be interesting Heidi to ask Doog's question to see if your surgeon does have an answer, because my surgeon couldn't answer that.
Jayne
The Eurospine link above talks about dehydration of the disc then this link [url]The Process of Disc Resorption[/url] suggests the macrophage theory:-
[INDENT]Just as your body would recognize and fight bacteria that try to invade a cut in your skin, so too does your body recognize the extruded nucleus pulposus from an annular tear as a material that should not come into contact with other bodily tissues. Your body’s immune system kicks in and uses macrophages – white blood cells that destroy pathogens – to break down the disc material until it can be completely resorbed by the body. With time, the annular fissure will close and heal.[/INDENT]
It's from a website I think SPINELF uses.
Why are we all told different things - it is so frustrating.........
Trust me I researched this to death last year and asked the surgeon so many questions, I don't think he knew what hit him!!!!
Jayne x
Hi Doog,
How did he know it would never go away though? My surgeon said in all honesty, they weren't actually clear what happens.
Jayne
Jayne, like you I had researched it to death but am still no clearer. I read somewhere that they did a study of patients and after 10 years those who didnt have surgery were at the same level as those who did - so much for surgery eh!
I think half the problem is that people who recover well from surgery and go onto lead a normal and active life tend not to post about it. My surgeon has apparently done 10,000 of these procedures - I have only seen his name mentioned once on these forums and that was a pre-op post - so that would indicate that the procedure may be successful - who knows?
As for differing advice, tell me about it. Same ward, same day, same operation, two different surgeons - both of us patients told different things- what you can do / cant do..its crazy
I have been told by my surgeon that it is unlikely to fix itself and that even with the operation there is no guarantee that it won’t return at a later date (so I wonder what’s the point?!) I will clarify this with him tomorrow and let you know what his response is.
What he did say is that it is unlikely to get worse....
Jayne, yes there are positions i can get in that make it less painful - standing and lying flat mostly. Like you I stand up often, I can still for more the 20 minutes when it is bad so i have no option.
I spent 6 hours of a 12 hour flight standing recently! I also sometimes need to stand when I am out for dinner - in the office I am constantly up and down. Like you I have research this topic to death and the more I read the more freaked out and indecisive I become….I have tried making lifestyle changes and they have gone so far to making it better. The more active I am (walking etc ) the better it seems it is…the problem comes when I try to relax, for example if I go on holiday, or go to the movies (this one is a total no go!). I even had to leave my bed and sleep on the sofa on several occasions as getting comfortable was impossible….how do you make changes with that? Yes still going with the Physio…I’m not giving up!!!
Doog, I can understand why you needed to make the decision in your circumstances, luckily I don’t have that pressure and work are being great. I think one of the main reason I am considering it is due to the fact I travel a lot with work, both long and short haul flights and several times a month – even on a trip over to Berlin I end up hanging out by the toilets as I can sit! Not even business class seats long haul are bearable when its bad….
I guess it doesn’t help that I have DDD with the discs above and below
One other questions, on my admissions sheet is state’s I will be having the following
‘Left L4/L5 Discectomy and L5 Nerver Root Decompression and and LA Injection into the skin’
Obviously I will be asking for more info on this tomorrow, but have you got any ideas what an LA injection into the skin is and what the root decompression is?? Is this standard with a discectomy?
Thanks guys
Hi 'Painintheback',
My question to you would be ; if the surgon said that he had desided not to operate on you how would you feel ???
I think, but maybe wrong, that there are no clear answers, thats why these forums are so helpful to all of us trying to make desisions !!
I have read post after post with the theme that all the info out there is inconclusive.
I am NOT an expert but have concluded that; a back operation can help and have positive outcomes, it can also help very little, there are also risks. Why the outcomes are so different there seems to be little answer wise !
I think that without a cristal ball you can not know what the best desision for your body is!!!!
However, you can deside if you as a person feels you should go ahead !! Sometimes others can take a persons need to talk about it and question it as it being the wrong thing for you to do!!!
As I sugested at the begining of this post,have a think, if the option to have it done was taken away would you feel relived or upset/angry. And, why.
I belive in 'gut feeling'. Good Luck
GREAT INFORMATIVE POSTS GUYS!!![]()
SPEAK SOON!
BEST OF LUCK FOR YOUR CONSULTATION HEIDI!
THAT LOOKS LIKE A 'VICIOUS' L4/5 DISC HERNIATION OF YOURS HEIDI! WHICH MEANS THAT YOU NEED TO GET YOUR QUESTIONS ANSWERED TOMMOROW!! DON'T LET THE SURGEON BULLY YOU INTO SILENCE OR INTO A QUICK EXIT!!
BEST WISHES
SPINELF
Hi Painintheback!
Just saw your post. Its brought me right back to that same place i was in before agreeing to have the operation. I really feel your stress, frustration and indecision. Its emotionally draining and even when you decide yes or no you'll still doubt yourself.
Firstly your scan shows a a decent rupture and the disc above and below bulging. So thats 3 possible causes of pain / back ache. With the rupture in the middle it'll put further pressure on the disc above and below in time as it shrinks.
Nobody can give you an answer only yourself. I reached ut on this forum and a personal message from another poster confirmed to me that you don't have to be carried into the hospital to get this done - its ok to get it done during a period where the pain subsided. If theres a pattern of it easing and returning etc. . If life has become limited by the condition and you feel its the right choice then go for it - if your not 100% convinced and ready for the 8wk rehab period then don't. The web is full of horror stories so my best advice is limit what you focus on.. First hand experience is best.
I met with 2 people who had a fusion and a disectomy beforehand. The disectomy was 10wks post surgery.
I guess i'll conclude with this. If this is stopping you working or living comfortably. As in a complete stop bed ridden. Then its time to consider surgery.
You have to now accept you have a back condition. Thats forever more and will need counter action - walking exercise etc
You have to very careful what surgeon you choose. Spend the time researching because your life is literally in there hands. Its a serious procedure.
I'm 8wks post op now. I was trimming hedges yesterday, i was at the gym swimming walking etc. Its always at the door but if you keep the walking and exercise going it works. I return to work tues 10th april. We'll see how that goes!!
Best of luck. Take your time and research and make the right decision.
Hi Heidi,
I left this forum alone for a year and now can't seem to leave the place! I just wanted to stop by and see if you had added an update from your surgeon.
Firstly, and I hope Ricky and Spinelf won't mind me saying, but just to reiterate we are not healthcare professionals and therefore certainly not qualified to report on your MRI scan. I found this link from the British Spine Surgeons Association very useful when trying to make sense of my scan [DLMURL="http://www.spinesurgeons.ac.uk/article.asp?article=29"]The Spine and MRI Scanning[/DLMURL]. We can all have bulging discs and the degree of prolapse does not necessarily correlate with the amount of pain and this is where the phrase "we treat the man (or woman!) not the scan" came from.
So please, please, please don't get hung up on the scan image. I really know how difficult it is not to and Doog is right it can almost convince you that you have to get it operated on now as the only option. But remember there are many people who have sciatica and have the same treatment as us, but never have a scan. My understanding is that the NHS won't even request an MRI before 12 weeks of symptoms and then there is often a waiting list - in my area another 5 weeks. There are others where a prolapsed disc is found coincidently on an MRI and the patient has no pain! So all in all the scan isn't the foremost consideration - it is how you feel and how it is impacting on your life that is important. Sorry rambling again......
I guess overall and I think Lizzy touched on it - is if you are happy that you have tried everything and say 3 months post op if you still had pain, you are comfortable that you won't turn round and think "I wish I had tried.........." or "I wish I had just given it a bit longer" and you can no longer live as you are and you trust your surgeon, then I guess it is time.
Some things to consider, some of this is for new patients looking at this thread. Other contributors please add/disagree/comment and remember I am NOT a healthcare professional - this is just how I see it:-
- Look at trusted websites like [url]EuroSpine - Sciatica[/url] to help you make an informed choice.
- prolapses can get better on their own. Nobody seems to know exactly how but dehydration or reabsorption via macrophages seem to play a part. It is not necessary for the disc to "go back in" (and it won't anyway). It just needs to pull back off the nerve.
- Nerves can repair themselves if damaged - don't get too panicked or pressured into quick surgery because of permanent nerve damage - that is rare. The only time emergency surgery is necessary is if you have Cauda Equina syndrome.
- Nobody seems to know how long it will take to get better - in most patients the most severe pain seems to have settled within 6 - 12 weeks. But other pain may continue for many months. My physio says up to 2 years, whether I had surgery or conservative treatment
- The bigger the prolapsed disc does not necessarily mean more pain. There are theories that bigger prolapsed discs may resolve more quickly because the body is more likely to recognise it as a problem and react to it. Comments from surgeons that "It's the biggest prolapse I have ever seen" are irresponsible.
- If your symptoms don't seem to be clearing ask your healthcare professional (Physio, GP or surgeon) if piriformis syndrome or nerve adhesions are a possibility and contributing.
- Physiotherapy (McKenzie exercises work for some) and talk to your Physio, I found mine much more knowledgeable than the GP and had experience of post surgical and conservative management of prolapsed discs and could give me stories of both recoveries. They also don't have any vested interest - they see you whether you have surgery or not! Remember you have to play an active part in physiotherapy and do your exercises regularly for it to work!
- Keeping gently active, keeping the spine moving helps blood flow and nutrients to get to it to help it heal. But listen to your body and rest when it tells you to. Walking is great but gently increase the amount you walk each day.
- Be prepared for a lifestyle change while healing - e.g. don't sit for too long, use a lumbar roll e.t.c. Prolonged sitting puts a lot of pressure on discs - so get up every so often to move around. Try not to bend too much, don't lift anything heavy (I was told max 5kg) and try not to twist.
- Drugs that don't heal but they help you keep active and do the physio exercises which does help with healing - amitriptyline, gabapentin or pregabalin (although they may have side effects). X ray guided epidural injection.
- Other pain relief - heat pads, TENS machines, acupuncture may be useful.
- Choose your surgeon carefully. If private or insurance think to yourself are they too keen to operate on me (very lucrative business) and conversely if NHS are they too reluctant. You would like to think that they would do the best for you, but targets, egos and empire building can play a part - don't be afraid to seek a second opinion.
- Think about the type of surgery - SPINELF has written many threads on this.
- Surgery is for pain in the leg only, it is not for pain in the back and may make back pain worse.
- Pilates can help improve core strength and stability - helping to reduce pain and prevent recurrence.
- Remember people do tend to post negative things rather than positives on websites. The successes tend to just get on with life. So don't be too scared by things you read on the internet!
Trusted websites I found useful:-
- European Spine Surgeons Website [url]EuroSpine - Sciatica[/url]
- British Association of Spine Surgeons Website [DLMURL="http://www.spinesurgeons.ac.uk/patientinfo.asp"]Patient Information[/DLMURL]
- NHS Choices - [url]Sciatica - NHS Choices[/url]
- Prodigy (this is what GP's use) [DLMURL="http://prodigy.clarity.co.uk/sciatica_lumbar_radiculopathy"]Prodigy - Clinical topic - Sciatica (lumbar radiculopathy)[/DLMURL]
Famous people who have suffered prolapsed discs:-
I found reading their stories really encouraging
Undergone surgery:-
- David Tennant (whilst in Hamlet!)
- Kate Silverton (BBC newsreader - possibly Cauda Equina - went on to have a baby).
Not had surgery:-
- Steve Redgrave - went on to win Olympic medals!
- Kelly Sotherton - two prolapsed discs - now doing the high jump as part of the Heptathalon for the Olympics!!
- Tony Blair - whilst PM
- David Walliams - whilst doing his Thames swim
Can anyone think of any more?
I may come back and add to this as I think of more. Sorry but after all I went through last year, I feel very passionate about things!!
I hope this helps someone.
Jayne xx
Heidi,
Hi, I was wondering how you were doing, if you had made any desisions ?
lizzy
Hi guys,
So sorry for not up dating sooner.
so after seeing my consultant I decided that I wasnt mentally ready to go ahead with surgery so cancelled and instead went ahead with a L5 nerve root block,despite being informed there was only a 20-30% chance of success. I have now had two of these within 6 weeks and I am disappointed to report that it hasn't worked.I had the last one on Thursday and was initially positive and convinced it had worked....but today as I sit here writing this I am still in pain.
I fear now my options are more limited than ever and the op it will need to be. I am seeing my consultant again in 2 weeks so guess that will be 'D' day.
Any last thoughts?!
Thanks
Heidi
Heidi
I fear now my options are more limited than ever and the op it will need to be. I am seeing my consultant again in 2 weeks so guess that will be 'D' day.
Any last thoughts?!
Hiya Heidi!
I am glad you made the decision you did, I think it was the right one!
I have had four nerve root bock injections, 2 were in the wrong place and completely
failed to work, the other 2 were injected in to the correct lumber level and worked completely, killing the pain 'fully' for 6 weeks and gave me an 11 week restbite from the worst of the symptoms.
So my thought is, that diagnosis for the location of your pain source is wrong and therefore the location of the pain releif injection was in the wrong place! It just makes sence to me!
Seriously think about getting a second opinion and more X-ray and MRI scans, I think more questions need to be asked of your Consultant when you see him, but don't be railroaded into a decision, make your own mind up, just as you did about the operation.
Best wishes and kind thoughts
SPINELF
Hi guys,
So sorry for not up dating sooner.
so after seeing my consultant I decided that I wasnt mentally ready to go ahead with surgery so cancelled and instead went ahead with a L5 nerve root block,despite being informed there was only a 20-30% chance of success. I have now had two of these within 6 weeks and I am disappointed to report that it hasn't worked.I had the last one on Thursday and was initially positive and convinced it had worked....but today as I sit here writing this I am still in pain.
I fear now my options are more limited than ever and the op it will need to be. I am seeing my consultant again in 2 weeks so guess that will be 'D' day.
Any last thoughts?!
Thanks
Heidi
Heidi
Hiya Heidi
HOW ARE THINGS NOW, ANY NEWS?:confused:
We Look forward to hearing from you.
SPINELF

